View from the frontline of anaesthesia during COVID-19, July 2020 survey results
View from the frontline of anaesthesia during COVID-19
Between 30 June - 05 July 2020, the College conducted a survey to assess its members' views on the current preparedness to restart planned services.
Introduction
There is a growing expectation from clinicians, the NHS and the public to return to a ‘normal’ service as soon as possible, and to ‘catch up’ with cases postponed during the COVID-19 peak. The College understands that there is a pressing need to return to ‘normal’ activity, and that unintended harm may be caused by not doing so. With this in mind, the College welcomes the Government’s recent announcement of £3 billion of additional funding to help the NHS prepare for winter. However, returning to ‘normal’ surgical activity will be challenging so, in May 2020, the College published, in partnership with the Association of Anaesthetists, Intensive Care Society and Faculty of Intensive Care Medicine, a strategy on the restoration of planned surgery.
Delivering care safely, efficiently and sustainably, means taking into account the staffing, environment and equipment needed to operate, and the impact of caring for COVID-19 patients on postoperative critical care capacity. Planned activity must match a realistic assessment of the NHS staff and resources needed. Across four categories, Space, Staff, Stuff and Systems, the strategy offers a RAG-rating for readiness to return to normal activity. Between 30 June-05 July, we asked the College’s members to assess current readiness against the four categories. 334 members from across the UK completed our third COVID-19 membership survey, and this briefing outlines their views and offers a set of recommendations to complement national guidance and offer a way forward in this ‘new normal.’
Who is this briefing for?
Civil servants, ministers, parliamentarians, College fellows and members, clinical directors, NHS, public health and social care organisations across the UK, our partners, and the public.
What is this briefing for?
- To offer a headline assessment of the NHS’s current preparedness to restore planned services, and what our members think needs to happen to support a full restoration.
- To represent the voice of the College’s members on the issues that matter most to them during COVID-19, and to feedback their views as expressed in the COVID-19 survey.
- To support civil servants, ministers, parliamentarians and key decision makers to understand, and mitigate, the pressures faced by anaesthetists during COVID-19.
- To highlight the role of anaesthetic teams in managing COVID-19 and treating COVID-19 patients; and to encourage decision-makers and the public to champion the profession.
View all survey findings and key recommendations in one glance
Key findings
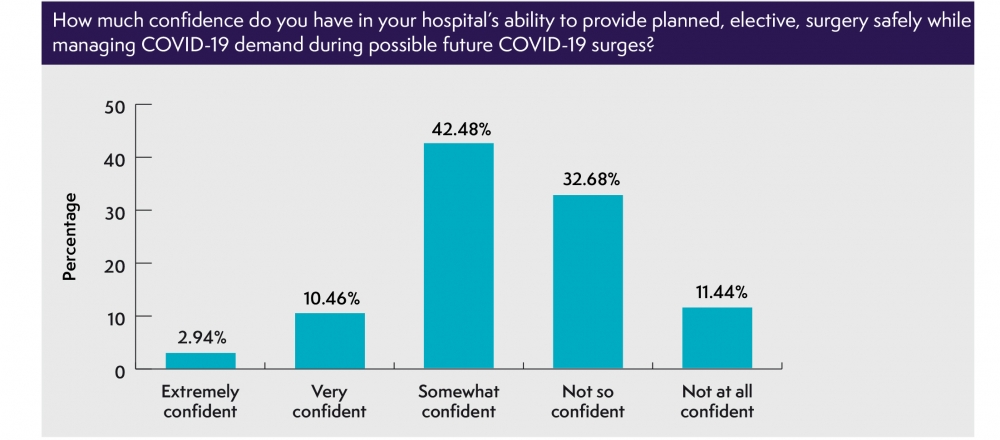
- 44% of respondents are not confident in their hospital’s ability to provide planned surgery safely while managing COVID-19 demand during future surges.
- Nearly two-thirds of respondents (64%) have, to some extent during the last month, suffered mental distress because of additional work related stress due to COVID-19.
- Nearly nine in ten trainees (89%) strongly agree that the pandemic is affecting their training opportunities, career and professional development.
Key recommendations
- NHS Improvement should publish a new People Plan, with the investment and teeth needed to support staff welfare and wellbeing, build resilience and address inequality.
- NHS Improvement should identify, train and maintain the skills of cross-specialty ‘reservists’ who can support COVID-19 surges, and escalation plans should rapidly be made, with the support of the Medical Royal Colleges.
- The Government should make a commitment to additional, and sustainable, investment in the resources, facilities and staff needed to support a return to pre-COVID-19 activity.
- Hospitals and trusts may need to cohort specialist surgery on a regional basis; and there is merit in a ‘clean hospital’ approach. Other locations for managing planned surgery or COVID-19 care should be considered, with sufficient resources that are separate from those within the NHS.
- Efforts should be made to support hospitals in ensuring that sufficient numbers of anaesthetic, theatre, perioperative care and ward staff are free to return to their routine work activities.
- A transparent, flexible, approach to re-scheduling assessments and teaching should be developed, with clear guidance on how missed learning opportunities will be delivered.
1. SPACE
Many hospitals have used operating theatres, Post-Anaesthesia Care Units (PACUs) and surgical ICUs to accommodate Level 2/3 patients. Normal surgical activity should not resume if they remain as temporary ICUs for logistic and Infection Prevention and Control (IPC) reasons.
- 44% of respondents aren’t confident in their hospital’s ability to provide planned, elective, surgery safely while managing COVID-19 demand during possible future surges.
- 39% of respondents don’t feel their hospital has the space required to provide elective surgery safely (e.g. PACUs, recovery rooms or ICUs) while managing surges.
- While 70% of respondents report that critical care occupancy in their hospital is now close to pre-pandemic capacity, nearly one in six (17%) report that it is not.
- While 70% of respondents report availability of postoperative critical care capacity in their hospital, nearly one in seven (15%) report that it is only to a small or to no extent available.
Recommendations
- Continued support of locations managing planned surgery or care of COVID-19 patients will be necessary e.g.: independent hospitals and Nightingale hospitals, matched by sufficient resources (separate from the NHS) needed to effectively deliver their work.
- Further expansion in critical care facilities may be required if coronavirus infection rates increase again or demand from other seasonal illness increases. We note the very low level of ICU bed provision in the UK compared with other parts of Europe.
- Temporary ICUs occupying key locations on the surgical pathway should be relocated, and normal surgical activity should not resume if theatres, PACUs and surgical ICUs remain as temporary ICUs for logistic and IPC reasons.
- Where it is not possible to ‘step down’ temporary ICUs, it must be recognised that this is not ‘business as normal’, and planning surgery should be undertaken in this context.
2. STAFF
A number of factors will affect staff capacity for some time to come, which need to be addressed to provide assurance of our ability to restore planned surgery.
- Nearly two-thirds of respondents (64%) have, to some extent during the last month, suffered mental distress because of COVID-19; while nearly one in four (24%) can’t take the time off they need to seek help or rest.
- Just over a third of respondents (34%) report a low/very low level of team morale, compared with nearly one in five (21%) the previous month; while those feeling ‘very well supported’ by their employer dropped from 27% in May to one in six in July (17%).
- During the recent peak, 43% of respondents were re-deployed to work in ICU. Of those, 29% have been unable to return to routine work activities.
- More than one in four respondents (26%) report that their employer is not properly remunerating them for clinical time owed for flexible working or additional hours under surge conditions.
- More than one in four respondents (26%) have been unable to access educational activities compliant with normal revalidation requirements during the past three months.
- Over one in six respondents (16%) don’t plan to take their accrued/deferred leave over the next 3-6 months (either because they’re unable to, are able to but plan not to, or have none to take); while over one in five (21%) are carrying it into next year.
“We have burned out our human resource. We need a period of rebuilding or patient harm will result”
Trainees
- Nearly nine in ten trainees (89%) report that their training opportunities have been affected, with 45% telling us that their local employers/education providers haven’t developed mitigation plans, and over three in four (76%) losing out on clinical learning.
- 95% of trainees report that on call rotas have changed during the pandemic, with 60% reporting that they haven’t returned to normal, one in three (33%) reporting that on call rotas don’t have a normal number of trainees available, and nearly one in three (32%) reporting that where on call rotas have changed, this hasn’t been with their agreement.
- More than one in three trainees (35%) have not been informed in a timely manner of changes impacting on their teaching, exams and progression, while nearly one in five (17%) haven’t been able to access their curriculum remotely and more than one in five (22%) report that their annual review was not delivered on time.
“The prospect of exams is increasingly stressful. Now the peak has passed I have to [study] but I’m exhausted, [and] lack proper revision courses and regional teaching”
Recommendations
- There must be remediation of the potential for fatigue and stress from shift working, long hours and dealing with death, time owed for Bank Holidays and leave, sickness from coronavirus or other illnesses, and inadequate access to educational activities compliant with normal revalidation. This will require a People Plan with teeth and investment, to support staff welfare and wellbeing, build resilience and address inequality.
- Substantial expansion of critical care staffing may be needed to address pandemic cross-cover, release theatre and perioperative care staff and provide future resilience. Identification, training and skill upkeep of cross-specialty ‘reservists’ who can support COVID-19 surges and escalation plans should be rapidly made. We welcome the ongoing work being undertaken by the Faculty of Intensive Care Medicine on the development of enhanced perioperative care as a positive way forward.
- Efforts should be made to ensure that sufficient numbers of anaesthetic, theatre, perioperative care and ward staff are free to return to their routine work activities.
- Clinicians must be paid for time owed for flexible working under surge conditions.
- All hospitals should have an explicit plan for rescheduling training opportunities (including assessments) that were lost. Trainees need a transparent and flexible approach to re-scheduling assessments and teaching, to be informed in a timely manner of changes to teaching, examinations and progression, and clear guidance on how missed learning opportunities will be delivered.
3. STUFF (EQUIPMENT)
COVID-19 infection will remain in the community for months, if not years, and it is essential that sustainable supplies of the right equipment must be in place at the right time to support our clinicians, the wider health and care team and their patients.
- One in five respondents (20%) report a lack of sufficient IPC measures in place in their hospital to prevent staff infecting surgical patients; with nearly one in five (17%), respectively, to prevent surgical patients infecting staff.
- While 72% of respondents report that, in their hospital, there are sufficient stocks of PPE available for effective critical care and planned surgery, over one in ten (15%) report that there are only a small or no sufficient stocks of PPE available.
- While nearly two-thirds of respondents (61%) report that equipment for use in surgical care pathways (e.g. anaesthetic equipment or infusion pumps) that was redeployed to critical care has been returned to its normal location, 15% report that this is not the case.
Recommendations
- Equipment used in surgical care pathways to support a critical care surge response will need to be returned to its normal location and usage before elective activity can restart.
- The IPC measures (and stocks, e.g. PPE) needed for current and possibly increased ward and critical care management must be available before any planned surgery restarts.
- Securing adequate drug stocks for expected critical care and emergency anaesthetic activity is essential to any return to planned surgical activity.
- Critical care facilities should be assessed on a speciality basis, e.g. if renal replacement therapy facilities remain saturated after ICU capability is restored, this will impact on the ability to restore planned cardiac, major vascular and high-risk general surgical work.
4. SYSTEMS
A return to pre-COVID-19 activity levels will be difficult without additional investment in resources, facilities, staff, time – and IPC measures.
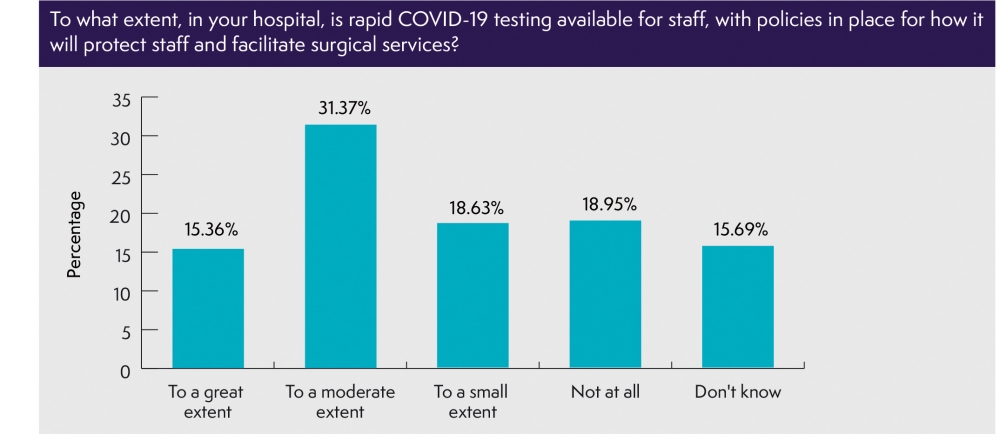
- Over a third of respondents (38%) report that rapid COVID-19 testing is only to a small or to no extent available for staff, with policies in place for how it will protect patients to facilitate surgical services; with only one in five (26%) respectively for patients.
- While nearly four in five respondents (79%) report that COVID-19-positive and negative pathways for surgical care have been planned and implemented in their hospital; nearly one in six (16%) report that they have been planned but not implemented.
- 67% of respondents agree that standard operating procedures for surgical services, operating theatres and critical care need review and adjustment.
- 42% of respondents report that, in their hospital, anaesthetic services supporting theatre activity, eg preoperative assessment, acute pain services and perioperative care, are only to a small extent or not at all working to pre-COVID-19 levels.
Recommendations
- Additional investment in resources, facilities and staff, e.g. IPC processes will be necessary to support a return to pre-COVID-19 levels of activity.
- Maximising equipment, postoperative care and other resources may mean specialist surgery will need to be cohorted on a regional basis; and there is potential merit in a ‘clean hospital’ approach of cohorting by site, particularly to address public concern.
- Maximising surgical activity requires streaming patient flows using patient shielding before admission and testing such that COVID-19-positive and -negative pathways are created; and consideration should be given to streaming surgical, anaesthetic and theatre team staff, separating teams doing elective work form those doing emergency/on call work.
- All Standard Operating Procedures for surgical services, operating theatres and critical care will need careful review and adjustment as necessary.
For more information, please contact:
Mark Weiss, Head of Policy and Public Affairs, mweiss@rcoa.ac.uk
Elena Fabbrani, Policy and Patient Information Manager, efabbrani@rcoa.ac.uk
