Risks and side effects – headache after a spinal or epidural anaesthetic
About this leaflet
This leaflet is about the risk of developing a severe headache called a post-dural puncture headache after a spinal or epidural anaesthetic injection. It explains how it can happen and what can be done about it.
Spinal and epidural anaesthetics are types of regional anaesthetics. Regional anaesthetics are injections that numb a specific part of the body. For spinal and epidural anaesthetics, the anaesthetic injection is given between the bones in your back to numb the lower part of the body.
More information on regional anaesthetics can be found on our Patient information leaflets and video resources webpage.
More information on the use of epidural and spinal anaesthetics during childbirth can be found on the LabourPains website.
What does the headache feel like?
- The headache can be severe.
- You tend to feel it at the front or the back of your head.
- It can feel worse when sitting or standing and better when lying down.
- You might have neck pain or stiffness.
- You might feel sick and develop sensitivity to light.
- It usually starts between one day and one week after the anaesthetic.
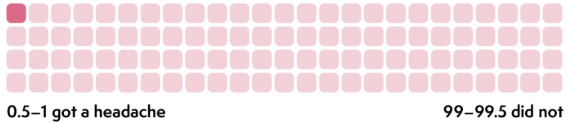
How likely is it to happen?
Out of every 100 people
Patients who have a spinal or epidural for childbirth are more likely to develop a dural puncture headache.
These numbers come from research studies. You can find out about the research we used in our Spinal anaesthesia and risk evidence table.
What causes a dural puncture headache?
The brain and spinal cord are contained in a bag of fluid called the ‘dural sac’. A dural puncture headache happens if some of this fluid leaks out and the pressure around the spine and brain falls.
For an epidural, a needle is used to inject local anaesthetic just outside the dural sac. If the needle accidentally pierces the sac, a small hole is made, through which fluid can leak out.
When a spinal injection is given, a very fine needle is deliberately inserted through the dural sac. Normally this does not cause any problems but, in some cases, this can lead to fluid leaking out.
If you sit or stand up, the pressure of the fluid in the dura can fall even further. This can make the headache feel worse. If you lie down, the pressure increases and the headache can feel better.
What happens if I develop a headache after a spinal or epidural?
If you develop a headache, there are some things that you can do yourself initially:
- take over-the-counter pain relief such as paracetamol or ibuprofen
- drink plenty of fluids
- caffeinated drinks can help (coffee, tea, cola)
- avoid straining or lifting anything heavier than your baby
- lying down can help relieve the pain.
You should contact your midwife or hospital team or visit an emergency service if:
- your headache does not get better after taking over-the-counter pain relief
- the headache gets worse
- you are not able to care for your baby or do normal everyday tasks
- you have problems with your vision and hearing
- you feel sleepy, sick or confused.
You may be advised to return to hospital so that the healthcare team can assess you and ensure that there are no other serious causes for your headache. If a dural puncture headache is suspected, one of the anaesthetists will review you. If you have a headache after childbirth, you can usually keep your baby with you in hospital.
How is a dural puncture headache treated?
If the healthcare team thinks that you have a dural puncture headache and pain-killers do not help, you may be offered an epidural blood patch. The procedure is very similar to having an epidural. Evidence shows that an epidural blood patch is more effective if carried out 48 hours or more after the severe headache starts.
For an epidural blood patch, a little of your own blood is taken from your arm and injected into your back. The blood seals the hole in the dura and stops more fluid from leaking out. This helps the pressure to build back up so that the headache improves. You will need to lie flat for at least 1–2 hours after the procedure.
How well does an epidural blood patch work?
Out of every 100 people who had a blood patch
What are the side effects and risks from an epidural blood patch?
- The procedure might feel uncomfortable
- There may be bruising where the needle goes in
- It can cause backache and stiffness, which can last for a few weeks
- It could cause another puncture to the dura, which could make the headache worse. This risk is the same as having a dural puncture headache in the first place.
|
You should seek medical help immediately from your midwife or visit A&E if you have had an epidural blood patch and you:
|
This leaflet has been produced by Leila Finikarides for the RCoA, in collaboration with patients, anaesthetists and patient representatives of the RCoA.
Disclaimer
We try very hard to keep the information in this leaflet accurate and up-to-date, but we cannot guarantee this. We don’t expect this general information to cover all the questions you might have or to deal with everything that might be important to you. You should discuss your choices and any worries you have with your medical team, using this leaflet as a guide. This leaflet on its own should not be treated as advice. It cannot be used for any commercial or business purpose. For full details, please click here.
Second Edition, May 2025
This leaflet will be reviewed within three years of the date of publication.
© 2025 Royal College of Anaesthetists
This leaflet may be copied for the purpose of producing patient information materials. Please quote this original source. If you wish to use part of this leaflet in another publication, suitable acknowledgement must be given and the logos, branding, images and icons removed. For more information, please contact us.