Epidural anaesthetics: risks and side effects
About epidurals
An epidural is a type of anaesthetic where a very thin plastic tube (catheter) is put in your back. Your anaesthetist uses the catheter to give you pain medicines to relieve pain or numb the lower part of your body. The catheter stays in your back and you can have more pain relief if you need it.
Epidurals are often used as pain relief during childbirth to make contractions less uncomfortable. You can get more information about epidurals for childbirth on the LabourPains website.
Epidurals can also be used for surgery and pain relief after surgery. You can read more about epidurals for surgery in our leaflet Epidural anaesthesia during and after surgery.
About risk and epidurals
Everyone is different and it is not possible to know who will experience a side effect or risk.
Knowing about risks can help you discuss options with your healthcare team and make informed decisions about your care or birth plan.
The risks in this leaflet are averages obtained from research studies. You can find out about the research that we used in our epidural anaesthesia and risk evidence table.
Your risks might be higher or lower than these numbers. If you are thinking about having an epidural for surgery, your anaesthetist will discuss with you the risks that are more likely or significant for you.
If you’re thinking about having an epidural during childbirth, you might not meet the anaesthetist until you’re in labour. Since labour can be unpredictable, you might decide to have an epidural even if you hadn’t planned to. Whether an epidural is part of your birth plan or not, reading this leaflet and others on the LabourPains website can help you prepare for the unexpected and think about any questions you might have.
Risk and epidurals during childbirth
According to the latest evidence, epidurals:
- do not make you more likely to need a caesarean birth
- do not make the use of ventouse or forceps more likely
- do not make your baby drowsy or cause them long-term harm
- do not cause backpain after childbirth.
Choosing an epidural for pain relief during labour may help lower the chance of serious complications, such as heavy bleeding (haemorrhage), infections, blood clots or the need for intensive care.
Epidurals can make childbirth safer if:
- you live with obesity
- you have existing health problems
- you are expecting more than one baby
- your baby is premature (born early).
What happens if the epidural does not work?
Epidurals do not always work as well as they should and sometimes they do not work at all. They take about 20 minutes to set up and up to 30 minutes before you feel the full effect. If it is not working well for you, tell your midwife or anaesthetist. They can:
- give you more anaesthetic through the catheter
- ask you to change your position
- move the catheter to a different place in your back (re-siting)
- suggest a different type of anaesthetic.
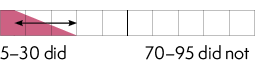
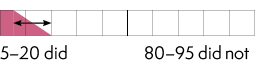
Out of 100 people who had an epidural during labour
About 10 needed additional pain relief as well as the epidural – 90 did not
About 5 had to have the epidural re-sited – 95 did not
Risks and side effects associated with epidurals
| These numbers are out of every 100 people who had an epidural | |
| What happened? | For how long? Can it be treated? |
|
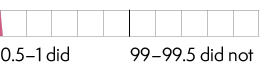
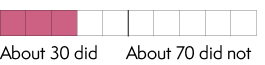
Headache (post-dural
|
It can happen between one day and one week after the epidural. It can be mild and get better within a few days with over-the-counter pain relief, or it can be severe and require treatment in hospital. You can get more information about post-dural puncture headaches from our leaflet Headache after a spinal or epidural anaesthetic. How many?
|
|
Fever |
It can happen in the hours after an epidural and last for a few days. Your healthcare team may offer you antibiotics if it is caused by an infection. How many? |
|
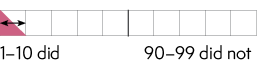
Low blood pressure |
It can happen immediately and last for a few hours soon after the epidural. It can make you feel sick, dizzy or drowsy. Your healthcare team can give you medicine to improve your blood pressure. How many? |
|
Feeling sick (nauseous) |
It can happen immediately and last for a few hours soon after the epidural. Your healthcare team can give you anti-sickness medicines if it happens. How many? |
|
Itching |
It can happen immediately and usually wears off after a couple of hours. Your healthcare team can give you medicine to treat the itching. How many? |
|
Difficulty passing urine |
You might not be able to feel if you need to go to the toilet after an epidural. The healthcare team sometimes recommends a urinary catheter, a thin tube to drain the urine directly from your bladder. This might stay in until the next day.
|
The risks below are rare.
| These numbers are out of every 1,000 people who had an epidural | |
| What happened? | For how long? Can it be treated? |
|
Local anaesthetic toxicity |
These are serious complications. Your team will treat you quickly if they happen. How many? About 1 did – About 999 did not
|
| These numbers are out of every 20,000 people who had an epidural | |
|
Weak, numb, tingly leg,
|
Temporary damage: (days or weeks) and normally gets better by itself. How many? 8 did – 19,992 did not Permanent damage How many? About 1 did – About 19,999 did not You can get more information from our leaflet Nerve damage after a spinal or epidural anaesthetic. |
| These numbers are out of every 50,000 people who had an epidural | |
|
Meningitis symptoms
|
Meningitis infection can happen days or weeks after the epidural. This can be treated with antibiotics. How many? 1 did – 49,999 did not
|
| These numbers are out of every 200,000 people who had an epidural | |
|
Infection in or around |
It happens days or weeks after the epidural. It is treated with antibiotics or sometimes surgery to drain an abscess. How many? 2 did – 199,998 did not
|
|
Blood clot around the |
This is a serious complication which may require emergency surgery. It can cause leg paralysis if not treated quickly. How many? 1–2 did – 199,998 did not
|
| These numbers are out of every 500,000 people who had an epidural | |
|
Becoming paralysed |
How many? 2 did – 499,998 did not
|
Disclaimer
We try very hard to keep the information in this leaflet accurate and up-to-date, but we cannot guarantee this. We don’t expect this general information to cover all the questions you might have or to deal with everything that might be important to you. You should discuss your choices and any worries you have with your medical team, using this leaflet as a guide. This leaflet on its own should not be treated as advice. It cannot be used for any commercial or business purpose. For full details, please click here.
First Edition, September 2025
This leaflet will be reviewed within three years of the date of publication.
© 2025 Royal College of Anaesthetists
This leaflet may be copied for the purpose of producing patient information materials. Please quote this original source. If you wish to use part of this leaflet in another publication, suitable acknowledgement must be given and the logos, branding, images and icons removed. For more information, please contact us.